Scientists at Penn’s Institute for RNA Innovation pursue vaccines to stop celiac disease
Jax Bari, an 11-year-old from Philadelphia, shows me a photo of himself. It’s hard to look at; in it, he’s sprawled out on the bathroom floor, sad, exhausted. He says, just hours earlier, he had accidentally consumed gluten while out to eat with his family. What followed was hours of vomiting, diarrhea, and stomach pain.
That was April 2023, the time he’s felt the sickest from eating gluten. “For me, eating can be scary,” said Bari. He can’t go to a friend’s house, enjoy a birthday party, go out to eat with his family, or snack at after-school events without carefully reading food labels, asking a lot of questions, planning, and worrying that he’ll get sick again.
Bari is one of an estimated 3.3-million people in the United States who have celiac disease, a potentially life-threatening autoimmune disease where gluten, a protein in wheat, barley, and rye, causes damage to the small intestine. It’s different and more severe than gluten sensitivity, and it’s not just an allergy. Those with celiac disease cannot process gluten; they can have digestive issues, trouble absorbing the necessary nutrients their bodies need, and potentially lasting damage to their small intestine which can make those absorption issues chronic and lead to cancer.
New research published in the journal Clinical Gastroenterology and Hepatology in December confirmed the understanding that people with celiac disease are more likely to develop lymphoma and small bowel cancer, and also found people with the disease have increased risks of pancreatic, esophageal, gastric, and colonic cancers.
Currently, there’s no treatment for celiac disease aside from avoiding gluten. In situations where someone becomes really dehydrated, the only treatment is giving replacement fluids through an IV.
“I have to eat like everyone else, but there is always a chance that my food might have come into contact with gluten,” said Bari. “If there was a medicine that could allow me to eat gluten or even one that would help reduce my symptoms if I accidentally did, that would change my life.”
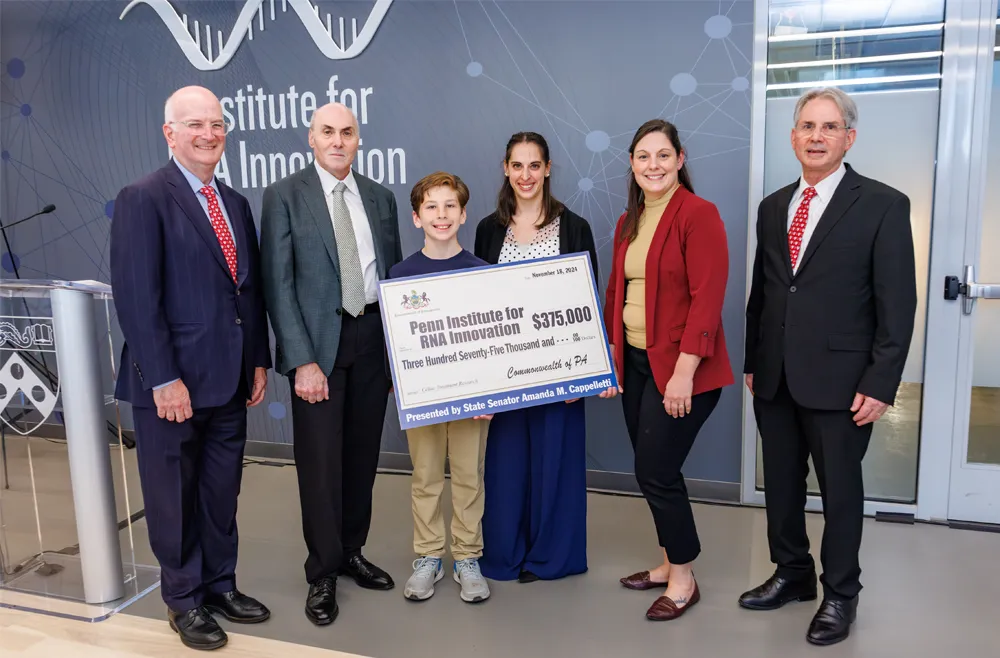
One possible answer to that life-changing question? New research is using messenger RNA (mRNA) led by Penn Medicine’s Drew Weissman, MD, PhD, the Roberts Family Professor of Vaccine Research and Jilian Melamed, PhD, research assistant professor of Infectious Diseases.
Subscribe to our newsletter
"*" indicates required fields